— Evidence is rated as insufficient to differentiate the net health benefit between ublituximab and other monoclonal antibodies; analyses suggest ublituximab and all currently available monoclonal antibodies labeled for MS would achieve common thresholds for cost-effectiveness if priced between $16,500- $34,900 per year, a range far lower than current market prices net of all rebates —
— At the January 20 virtual public meeting, ICER’s independent appraisal committee will review the evidence, hear further testimony from stakeholders, and deliberate over these treatments’ comparative clinical effectiveness, other potential benefits, and long-term value for money —
BOSTON, December 21, 2022 – The Institute for Clinical and Economic Review (ICER) today posted its revised Evidence Report assessing the comparative clinical effectiveness and value of the following treatments for multiple sclerosis (MS):
Monoclonal Antibodies
- natalizumab (Tysabri®, Biogen)
- ofatumumab (Kesimpta®, Novartis)
- ocrelizumab (Ocrevus®, Genentech)
- rituximab (Rituxan®, Genentech, and biosimilars)
- ublituximab (Briumvi™, TG Therapeutics)
Oral Therapies
- dimethyl fumarate (Tecfidera®, Biogen, and generics)
- diroximel fumarate (Vumerity®, Biogen)
- monomethyl fumarate (Bafiertam®, Banner Life Sciences)
- fingolimod (Gilenya®, Novartis)
- ozanimod (Zeposia®, Bristol Myers Squibb)
- ponesimod (Ponvory®, Janssen)
- siponimod (Mayzent®, Novartis)
- teriflunomide (Aubagio®, Sanofi)
“Multiple sclerosis is a burdensome condition, and individuals with MS manage declining function and neurologic symptoms such as weakness, fatigue, vision changes, pain, and balance problems for the rest of their lives,” said Jon Campbell, PhD, MS, ICER’s Senior Vice President of Health Economics. “ICER focused on evaluating the comparative benefits of currently available monoclonal antibody treatments and the emerging agent ublituximab, which has an expected FDA approval date later this month, against other first line disease modifying therapies (DMTs). All assessed DMTs demonstrate clinical benefits versus placebo, but there was insufficient evidence to differentiate between the benefit of ublituximab and other monoclonal antibodies. Our analysis also found that monoclonal antibodies would need to be priced considerably lower than they are now in order to meet traditional standards for cost-effectiveness.”
This Evidence Report will be reviewed at a virtual public meeting of the New England CEPAC (New England CEPAC) on January 20, 2023. The New England CEPAC is one of ICER’s three independent evidence appraisal committees comprising medical evidence experts, practicing clinicians, methodologists, and leaders in patient engagement and advocacy.
A draft version of this report was previously open for a four-week public comment period. The updated Evidence Report and voting questions reflect changes made based on comments received from patient groups, clinicians, drug manufacturers, and other stakeholders. Detailed responses to public comments can be found here.
Key Clinical Findings
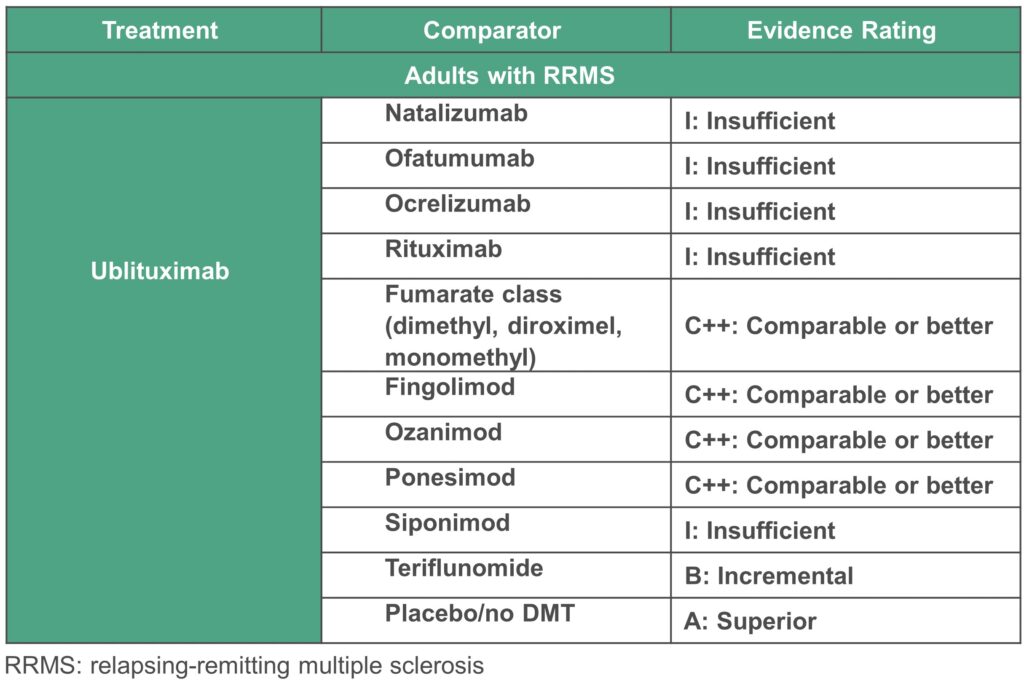
ICER found insufficient evidence to differentiate the net health benefit of ublituximab compared with other monoclonal antibodies. Ublituximab was judged to be comparable or better to oral DMTs in reducing annualized relapse rate (ARR) and confirmed disability progression (CDP). Based on head-to-head trial data, we had higher certainty that ublituximab provides a small net health benefit over teriflunomide. ICER did not have sufficient evidence to rate ublituximab versus siponimod due to differences in trial populations.
Key Cost-Effectiveness Findings
Because the clinical evidence was insufficient to differentiate between the monoclonal antibodies, we present one health-benefit price benchmark (HBPB) range across all modeled monoclonal antibodies (rather than a separate range for each intervention). Ublituximab, natalizumab, ofatumumab, and ocrelizumab will achieve common thresholds of cost-effectiveness if priced between $16,500- $34,900 per year.
ICER’s HBPB is a price range suggesting the highest US price a manufacturer should charge for a treatment, based on the amount of improvement in overall health patients receive from that treatment, when a higher price would cause disproportionately greater losses in health among other patients in the health system due to rising overall costs of health care and health insurance. In short, it is the top price range at which a health system can reward innovation and better health for patients without doing more harm than good.
About ICER
The Institute for Clinical and Economic Review (ICER) is an independent non-profit research institute that produces reports analyzing the evidence on the effectiveness and value of drugs and other medical services. ICER’s reports include evidence-based calculations of prices for new drugs that accurately reflect the degree of improvement expected in long-term patient outcomes, while also highlighting price levels that might contribute to unaffordable short-term cost growth for the overall health care system.
ICER’s reports incorporate extensive input from all stakeholders and are the subject of public hearings through three core programs: the California Technology Assessment Forum (CTAF), the Midwest Comparative Effectiveness Public Advisory Council (Midwest CEPAC), and the New England Comparative Effectiveness Public Advisory Council (New England CEPAC). These independent panels review ICER’s reports at public meetings to deliberate on the evidence and develop recommendations for how patients, clinicians, insurers, and policymakers can improve the quality and value of health care. For more information about ICER, please visit ICER’s website.
