— White bagging, brown bagging, and site of service policies developed by payers can reduce significant markup costs for clinician-administered drugs but have sparked concerns and legislative action related to their impact on patients and providers —
— White paper evaluating best practices and potential policy reforms was informed by input from a diverse set of hospitals, provider groups, and payers —
Boston, April 19, 2023 – The Institute for Clinical and Economic Review (ICER) has published a new White Paper in collaboration with researchers at NORC at the University of Chicago: “White Bagging, Brown Bagging, and Site of Service Policies: Best Practices in Addressing Provider Markup in the Commercial Insurance Market.”
The White Paper examines the efforts of payers to manage drug markups by implementing white bagging and brown bagging policies to shift the drug purchasing channel from providers to specialty pharmacies, as well as site of service policies requiring patients to receive treatment at lower-cost sites of care. The Paper examines the existing evidence and conflicting positions of payers and provider groups on how these policies affect patient safety, equitable access to care, and overall costs in the healthcare system. Potential best practices and associated policy reforms are examined for their relative advantages and possible unintended consequences.
“The high cost of specialty pharmaceuticals can now be seen driving change across the health care system,” said Steven Pearson, MD, MSc, President of ICER. “Provider markup is one link in the complex chain that can lead to unnecessarily high costs. Payers therefore have both a business interest and a stewardship responsibility to try to wring out unnecessary markup costs, and so it is no surprise that they have been increasing their efforts to move where possible away from the ‘buy-and-bill‘ system that has been the bedrock of reimbursement for many specialty drugs and is at the root of high provider markup costs. White bagging, brown bagging policies, and site of service policies are all part of this effort. There are approaches to the design and implementation of these policies that are more likely to reduce markup while being mindful of the risk for patient harm that include serious concerns about disproportionate effects for people in disadvantaged communities. Sound business practice and policymaking should aim to balance possible savings from reducing markup with thoughtful consumer protections and measures to improve transparency that can address the challenges that these policies may create for seriously ill patients.”
This White Paper went through several iterations following ICER’s Policy Summit in December 2022. At that meeting, policy leaders from leading provider groups joined with ICER’s Policy Leadership Forum (PLF) to discuss a preliminary draft, debate the policy recommendations, and provide suggestions for revisions to the paper. None of the individuals involved in this meeting, nor their organizations, should be assumed to support any part of this report, which is solely the work of the ICER team and its affiliated researchers.
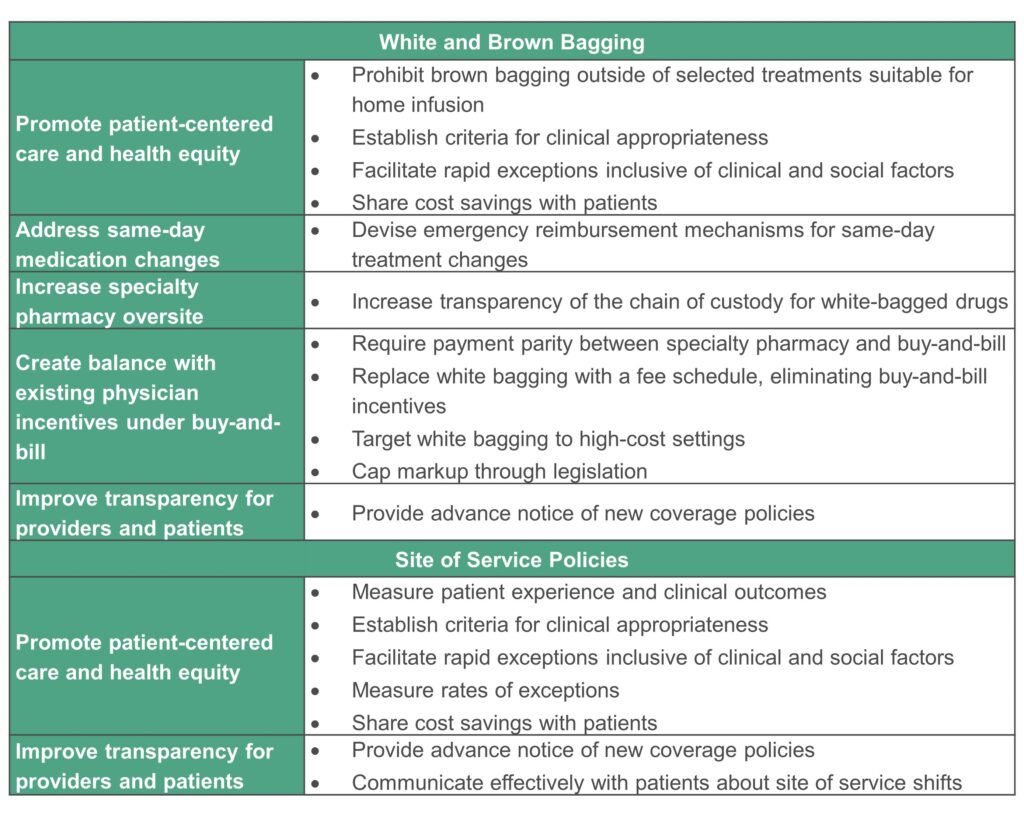
The White Paper analyzes the potential policy goals and associated best practices and reforms below:
ICER develops annual white papers in collaboration with the ICER Policy Leadership Forum. Previous papers have addressed topics such as Strengthening the FDA’s Accelerated Approval Pathway, Cornerstones of ‘Fair’ Drug Coverage, Reforms to Orphan Drug Development, Pricing, and Coverage, and Alternative Models for Pharmaceutical Rebates.
About ICER
The Institute for Clinical and Economic Review (ICER) is an independent non-profit research institute that produces reports analyzing the evidence on the effectiveness and value of drugs and other medical services. ICER’s reports include evidence-based calculations of prices for new drugs that accurately reflect the degree of improvement expected in long-term patient outcomes, while also highlighting price levels that might contribute to unaffordable short-term cost growth for the overall health care system.
